How Glycemic Load Affects Blood Sugar Spikes
Managing blood sugar is easier when you understand glycemic load (GL). Unlike glycemic index (GI), which measures how fast a food raises blood sugar, GL factors in portion size and carbohydrate content, offering a clearer picture of how meals impact glucose levels.
Key Takeaways:
- High-GL foods (GL of 20 or more) cause rapid blood sugar spikes, leading to energy crashes and hunger. Examples: white bread, instant rice, sugary cereals.
- Low-GL foods (GL of 10 or less) create steady energy by slowing glucose absorption. Examples: lentils, nuts, non-starchy vegetables.
- Pairing carbs with fiber, protein, or fats helps reduce GL and stabilize blood sugar.
- Smaller portions, meal timing (eating earlier in the day), and food swaps (e.g., quinoa instead of white rice) can help manage blood sugar more effectively.
Why it matters: Frequent blood sugar spikes increase the risk of insulin resistance and type 2 diabetes. Choosing low-GL foods supports long-term metabolic health, reduces inflammation, and helps maintain stable energy levels.
How to stop glucose spikes after meals. The Glycaemic Load
How High and Low Glycemic Load Foods Affect Blood Sugar
The glycemic load of food plays a key role in predicting blood sugar changes, helping you make better choices for consistent energy throughout the day.
Blood Sugar Response: High-GL vs. Low-GL Meals
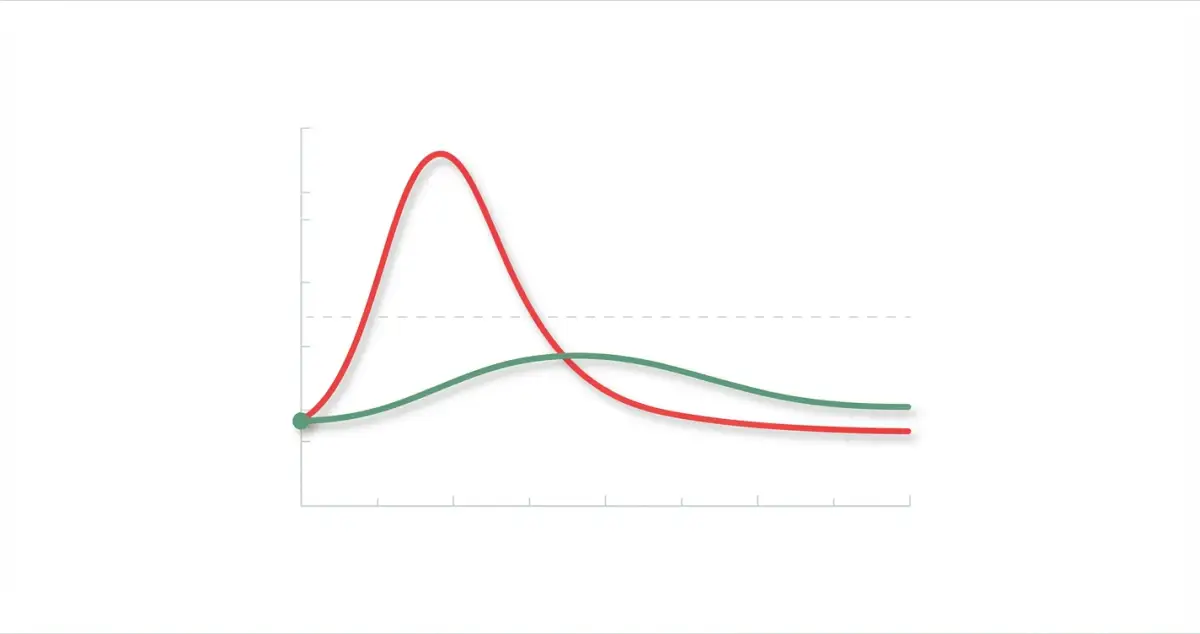
Meals with a high glycemic load (GL) can cause your blood sugar to rise rapidly. Think of a breakfast with white toast and jam - this kind of meal can lead to a quick spike in blood sugar, followed by a sharp drop soon after. This rollercoaster effect can leave you feeling drained and hungry again not long after eating.
In contrast, low-GL meals lead to a slower, more controlled rise in blood sugar. This gradual increase allows for a steadier release of insulin, which helps keep blood sugar levels balanced over a longer period.
Effects on Energy Levels and Hunger
These blood sugar shifts have a direct impact on how energetic and full you feel. High-GL foods often trigger what’s known as a “spike and crash” effect. You get an initial burst of energy, but it’s short-lived, followed by fatigue and a return of hunger. This cycle can make it harder to avoid cravings and maintain steady energy throughout the day.
Low-GL meals, on the other hand, provide more consistent energy. By keeping your blood sugar stable, they help you feel fuller for longer and maintain steady energy levels. Understanding these differences is essential for managing glycemic load effectively, which we’ll explore further in upcoming sections.
High and Low Glycemic Load Food Examples
Managing blood sugar levels starts with understanding which foods have a high or low glycemic load. Here’s a closer look at examples of both and the factors that influence these values.
High Glycemic Load Foods to Avoid
Foods with a glycemic load above 20 can cause sharp blood sugar spikes. Take white bread, for instance - just two slices can have a glycemic load of 20 to 25. Refined wheat pasta isn’t much better; a 1.5-cup serving can also fall into the high glycemic load category. Sugary breakfast cereals, like a bowl of corn flakes with milk, often exceed a glycemic load of 20, which might explain why you’re hungry again soon after eating. Instant white rice is another example, with one cup typically having a glycemic load in the low 20s.
Sweet snacks like donuts, cookies, and pastries are particularly problematic. These combine refined flour and added sugars, often pushing their glycemic loads beyond 25. Even some fruits can vary widely in glycemic load depending on portion size and ripeness. And don’t forget sugary beverages like sodas and sports drinks - they’re packed with sugar and can cause rapid blood sugar spikes almost immediately after consumption.
Low Glycemic Load Foods for Steady Blood Sugar
Low-glycemic foods, with a glycemic load under 10, can help keep blood sugar steady throughout the day. Non-starchy vegetables are great choices - 1 cup of broccoli has a glycemic load of about 1, and spinach has even less. Nuts and seeds are also excellent options. For example, an ounce of almonds (roughly 23 nuts) has a negligible glycemic load, while walnuts and sunflower seeds provide healthy fats and protein with minimal impact on glucose levels.
Whole grains, when eaten in moderation, can also be low-glycemic. A half-cup of cooked quinoa has a glycemic load around 9, and the same portion of steel-cut oats is about 7. Unsweetened plain Greek yogurt is another smart choice, with a 6-ounce serving typically having a glycemic load of around 3. Berries are naturally low-glycemic, too - a half-cup of strawberries has a glycemic load as low as 1, while the same amount of blueberries comes in around 3. Lean proteins like chicken breast, fish, and eggs are virtually carbohydrate-free, meaning they have no glycemic load.
What Affects Glycemic Load in Foods
Several factors influence a food’s glycemic load beyond its carbohydrate content. Fiber, for instance, slows glucose absorption. An apple eaten with its skin has a glycemic load of around 6, while apple juice (8 ounces) can double that to about 12 due to the lack of fiber.
Processing, ripeness, and cooking methods also play a role. Instant oats have a higher glycemic load than steel-cut oats because processing breaks down the grain’s structure. Similarly, white rice has a higher glycemic load than brown rice, which retains its fiber-rich bran layers.
Adding healthy fats and proteins to a meal can lower its overall glycemic load by slowing glucose absorption. Portion size also matters - a smaller serving naturally reduces glycemic load. Combining foods with fiber, fats, or protein is a practical way to manage blood sugar effectively while maintaining a balanced diet.
How to Manage Glycemic Load and Reduce Blood Sugar Spikes
Keeping your blood sugar levels steady involves thoughtful food choices, controlled portions, and well-timed meals. Small, steady changes to your diet can make a big difference.
Food Pairing and Meal Planning Methods
Pairing certain foods together is a simple yet effective way to manage blood sugar. For example, combining high-carb foods with healthy fats, proteins, or fiber (like extra virgin olive oil, nuts, chicken, or fish) slows digestion, helping to prevent sharp sugar spikes.
Here’s another tip: eat fiber-rich vegetables, proteins, and healthy fats before diving into starchy foods. This approach can significantly reduce blood sugar surges after meals.
Vinegar and pickled foods can also be helpful. Adding just a tablespoon of vinegar to a high-glycemic meal - or eating pickled vegetables - can slow digestion and improve blood sugar control by delaying gastric emptying and blocking certain digestive enzymes.
When planning meals, think about simple swaps. For instance, instead of a full cup of rice, try splitting it into ½ cup rice and ½ cup of black beans, lentils, or chickpeas. These legumes are lower on the glycemic scale and help balance blood sugar levels.
Once you’ve got food combinations down, consider tweaking portion sizes and meal timing for even better results.
Portion Control and Meal Timing Tips
Portion sizes play a huge role in managing your glycemic load. Overloading your plate - even with healthy carbs - can lead to higher blood sugar levels.
Timing your meals matters too. Your body is most sensitive to insulin in the morning, so eating earlier in the day can work in your favor. Research suggests that delaying your first meal by just one hour could raise glucose levels by about 0.6% and increase insulin resistance by 3%. On the flip side, eating large, carb-heavy meals in the evening can spike blood sugar and reduce insulin sensitivity.
To keep things steady, aim to eat earlier in the day and avoid heavy, carb-loaded dinners. Starting your meals later in the day has also been linked to consuming more calories, carbs, sugars, and fats, which can increase the likelihood of blood sugar spikes.
The next step? Transitioning to a diet that naturally keeps your glycemic load low.
How to Switch to a Low-Glycemic Load Diet
Switching to a low-glycemic diet doesn’t have to be complicated - it’s all about making smart substitutions. Replace high-glycemic foods with lower-glycemic options and keep portions in check.
Start by choosing whole, unprocessed foods. For example, opt for whole grain oats instead of processed, flour-based products. Similarly, choose whole fruits over fruit purees. If you’re a banana fan, less ripe bananas are a better choice since they’re higher in resistant starch and fiber, which result in a lower glycemic response.
Experiment with grains like barley and bulgur, which are naturally lower on the glycemic index, and try cooking pasta al dente - it helps keep blood sugar rises more controlled compared to overcooked pasta.
Don’t forget to include fruits and dairy (or dairy alternatives) in your diet - they often have a lower glycemic index. Combine high-carb meals with fiber-rich foods like vegetables, legumes, whole grains, nuts, and seeds to further reduce blood sugar spikes.
To keep your daily glycemic load under 100, focus on low-glycemic foods and monitor how your body reacts to different combinations. Everyone’s response is unique, so some trial and error might be needed.
If you’re looking for extra support, tools like the Logi - Glycemic Index Tracker App can help you track your meals and find low-glycemic alternatives to make the transition smoother and more manageable.
Tracking Your Blood Sugar Response to Glycemic Load
Once you’ve got your meal planning strategies in place, the next step is tracking how your blood sugar responds to different foods. Why? Because everyone’s body reacts differently. Monitoring your glucose levels helps you figure out which foods keep things steady and which ones cause sudden spikes. This knowledge becomes your guide for managing glycemic load effectively.
When and How to Test Blood Sugar Levels
Start your day by checking your fasting blood sugar before eating or drinking anything besides water. A normal range is 70–99 mg/dL.
To understand how your body reacts to meals, test your blood sugar at key intervals after eating - 30 minutes, 1 hour, and 2 hours. These checkpoints help you capture the typical peak (usually within 30–90 minutes) and track when levels return to baseline. Keep a detailed log of your meals, noting portion sizes and corresponding blood sugar readings. Over time, this data will reveal patterns and help you make informed decisions about your diet.
Using Apps to Track Glycemic Load
Manual logs work, but apps make tracking a whole lot easier. For example, the Logi - Glycemic Index Tracker App simplifies the process with features like a meal glycemic load scanner. This tool gives you an instant estimate of how your food choices might impact your blood sugar.
The app also includes a daily tracker that helps you pinpoint connections between specific foods and glucose spikes. Plus, it offers suggestions for low GI/GL alternatives, making it easier to swap high-impact foods for healthier options.
Long-Term Health Benefits of Managing Glycemic Load
While the immediate perks of managing glycemic load are clear, the long-term effects are equally compelling. Making thoughtful choices about glycemic load not only helps stabilize blood sugar levels but also plays a role in protecting against chronic illnesses and promoting overall wellness.
Lower Risk of Chronic Diseases
Keeping glycemic load in check can significantly lower the risk of developing chronic conditions like type 2 diabetes and heart disease. By avoiding frequent blood sugar spikes, you reduce the likelihood of insulin resistance, a key factor in diabetes. Additionally, steady blood sugar levels can help curb inflammation, which is closely tied to heart health, and make it easier to manage weight by controlling appetite.
When your blood sugar remains stable, your pancreas isn’t overburdened with producing insulin, which supports its long-term function. Studies have even suggested that diets with a lower glycemic load are linked to a reduced risk of diabetes compared to those filled with high-glycemic foods. In essence, managing glycemic load serves as a building block for long-term health and resilience against chronic conditions.
Improved Metabolic Health Over Time
A diet focused on low-glycemic load foods can enhance insulin sensitivity and promote more efficient glucose processing. This means your body uses energy more effectively, avoiding the dramatic energy spikes and crashes that come with high-glycemic foods.
Over time, this steady energy flow supports better nutrient absorption and reduces stress on your pancreas, helping it maintain its ability to produce insulin as you age. While natural metabolic changes are inevitable with time, mindful food choices can play a crucial role in preserving metabolic health and ensuring consistent energy levels well into the future.
FAQs
How does the glycemic load of food affect blood sugar and long-term health?
The glycemic load (GL) of a meal significantly influences your blood sugar levels and overall well-being. Consistently consuming high-GL foods can lead to sharp spikes in blood sugar and increased insulin production. Over time, this pattern may contribute to insulin resistance, inflammation, and metabolic imbalances.
These disruptions are associated with a greater risk of chronic conditions like type 2 diabetes, heart disease, and even certain cancers. On the flip side, meals with a low glycemic load help keep blood sugar levels steady, promoting better energy balance and lowering long-term health risks.
If you’re looking for a simple way to track the glycemic load of your meals and make smarter food choices, tools like Logi – Glycemic Index Tracker App can be a great asset.
How can I add low-glycemic load foods to my meals to help control blood sugar levels?
Maintaining steady blood sugar levels can be easier by including low-glycemic load foods in your diet. Start with non-starchy vegetables like spinach, broccoli, and zucchini. Add legumes such as lentils and chickpeas for a hearty, nutritious boost. For fruits, go for options like berries, apples, and pears, which naturally have a lower impact on blood sugar.
When eating higher glycemic foods like rice or bread, pair them with fiber-packed vegetables, lean proteins, and healthy fats. This combination helps slow sugar absorption. Swap out refined grains for whole options like quinoa, steel-cut oats, or whole-grain bread. Incorporating nutrient-rich greens and legumes into your meals not only supports blood sugar stability but also provides lasting energy throughout the day.
How can I track and manage my glycemic load to avoid blood sugar spikes?
Managing your glycemic load plays a big role in keeping your blood sugar levels steady. Focus on incorporating foods with a low glycemic load into your diet - think non-starchy vegetables, whole grains, and legumes. At the same time, try to cut back on high glycemic load items like sugary snacks and refined carbohydrates. If this feels overwhelming, keeping a food diary or using tracking tools can simplify the process.
For example, apps like Logi are great for scanning meals, keeping tabs on glycemic load, and suggesting healthier alternatives that align with your goals. Combine these tools with regular blood sugar checks - whether through a glucose meter or a continuous glucose monitor - for even better control over your blood sugar levels.
Further Reading
Take control of your blood sugar
Scan your meals, track glycemic load, and see your patterns — all in one app.
Start Free Trial →