Managing diabetes just got easier. Research shows diabetes apps can help lower HbA1c by an average of 0.49%, making them powerful tools for daily health management. The best apps focus on three key features:
- Blood glucose tracking with real-time data and device integration (e.g., CGMs and smart pens).
- Meal insights like glycemic load scanners and low-GI food suggestions for better dietary decisions.
- Health reminders for medications, glucose checks, and self-care tasks, personalized to fit your schedule.
Apps that combine simple designs, accurate data, and personalized tools help users take control of their blood sugar levels and improve long-term outcomes.
Making Diabetes Care Easier with Technology
Core Features That Make Diabetes Apps Work
Research highlights three key features that set effective diabetes apps apart. These features work together to help users better manage their blood sugar levels and stay engaged with their health routines. They provide accurate data, guide dietary decisions, and deliver timely health reminders to create a well-rounded support system.
Blood Glucose Monitoring and Tracking
Real-time tracking is essential for logging blood sugar levels and identifying trends. This information helps users make smarter daily decisions about their diet, physical activity, and medication schedules.
Today’s tracking tools go beyond simple logs. They offer visual charts, trend analysis, and pattern recognition to help users spot changes before they escalate into serious issues. One standout feature is device integration, which 43% of user reviews cite as a top priority. By syncing with continuous glucose monitors (CGMs), smart pens, and other devices, these apps eliminate the hassle of manual data entry, making blood sugar management more seamless.
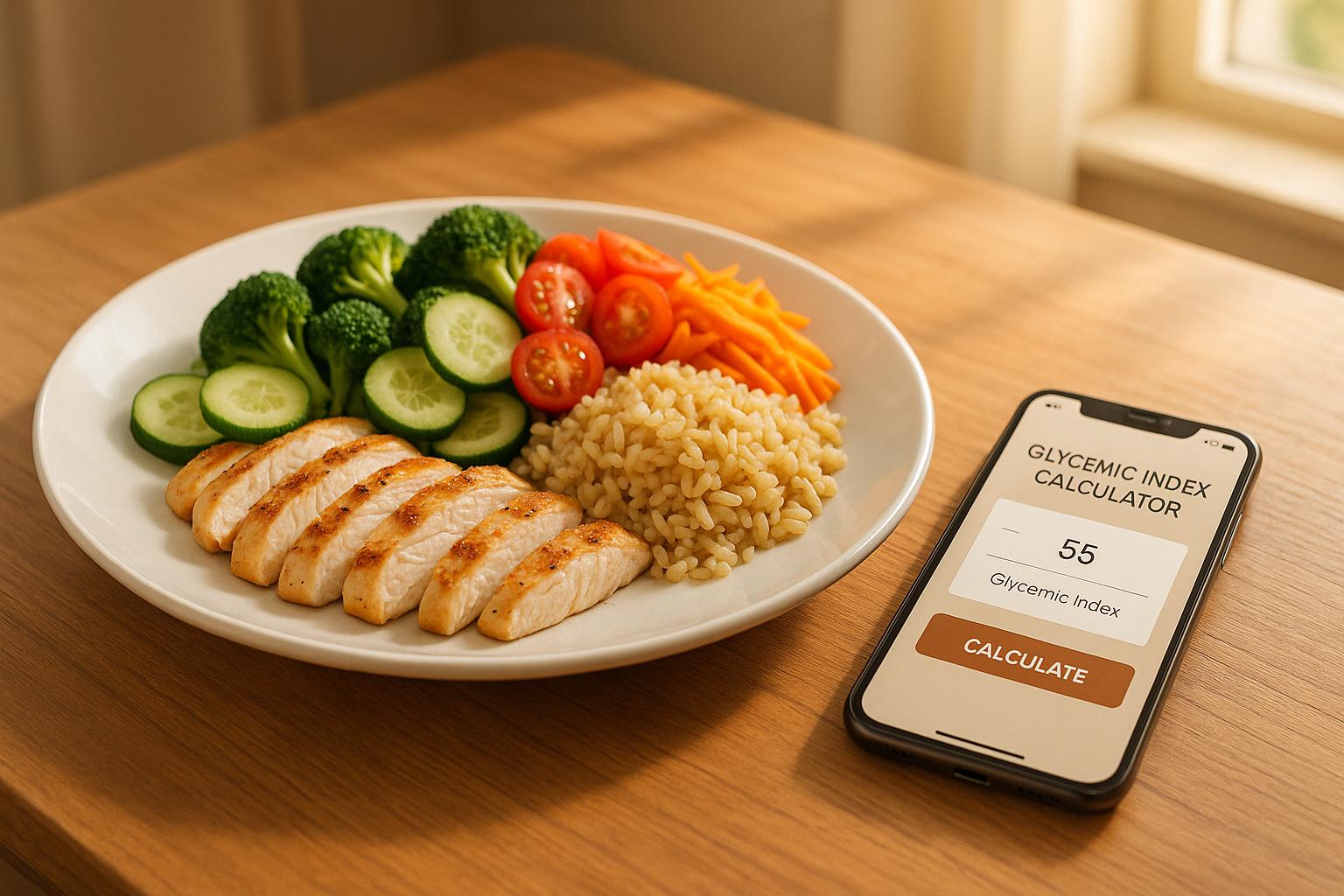
Dietary Logging and Meal Insights
Meal tracking and nutritional analysis are among the most impactful tools for managing diabetes day-to-day. These features help users understand how different foods influence their blood sugar levels.
Some apps include meal glycemic load scanners, which analyze food instantly to predict its impact on blood sugar. For example, Logi allows users to scan their meals and receive immediate feedback on how their food choices may affect glucose levels.
Effective apps also offer daily meal tracking that goes beyond counting calories. Users can log meals, review nutritional breakdowns, and gain insights into their eating patterns. This fosters healthier habits by connecting food choices to overall well-being.
Additionally, the best apps provide low GI/GL food alternatives finders that suggest healthier options tailored to individual needs. Instead of focusing on restrictions, these features empower users with practical alternatives that support stable blood sugar levels and sustained energy.
Medication and Health Reminders
Timely reminders play a crucial role in maintaining consistent self-care. Reminder systems in diabetes apps tackle one of the biggest challenges: staying on top of a care routine. Research shows that apps with these features improve adherence to treatment plans and self-management behaviors.
These reminders go beyond medication alerts. They include prompts for blood glucose checks, meal timing, doctor visits, and other health-related tasks. This reduces the likelihood of missed doses or skipped steps, which are vital for keeping blood sugar levels stable.
Personalized reminder scheduling enhances this feature by tailoring alerts to individual schedules, work routines, and lifestyle preferences. Customization makes it easier for users to follow through on their health management tasks.
Together, these three features - blood glucose tracking, dietary insights, and personalized reminders - address the core challenges of diabetes management. They help users understand their health status, make informed choices, and maintain consistent care routines.
Simple Design and Accurate Data
What sets a diabetes app apart - whether it becomes a daily health tool or gets abandoned after a week - often boils down to two key factors: ease of use and data reliability. Research consistently shows that straightforward interfaces and accurate data tracking lead to better health outcomes and higher user engagement.
Simple and Easy-to-Use Interfaces
The best diabetes apps follow design principles that prioritize clarity and ease of navigation, using plain language, clear visuals, and intuitive menus. Features like large touch targets, high-contrast text, and minimal layouts make these apps accessible and frustration-free. These thoughtful design elements allow users to log data and access insights with minimal effort.
Voice recognition for data entry and automatic uploads add another layer of simplicity, making these tools more accessible to a wide range of users. Interactive feedback, such as immediate confirmations, reassures users that their actions have been successfully recorded.
For example, Logi simplifies meal tracking with instant analysis through a single scan. It delivers health insights in a clear, digestible format that empowers users to make informed dietary choices without wading through complex data.
Studies consistently highlight that users value patient-friendly designs, which help sustain engagement over time. Apps that remove confusion and streamline user experiences make it easier for people to stick to their self-management routines. When paired with intuitive design, accurate data collection further enhances the app’s value.
Accurate Data Collection and Reporting
Reliable data tracking is the backbone of effective diabetes management. Monitoring blood glucose, meals, and medication with precision enables users and healthcare providers to identify trends, adjust treatments, and avoid complications.
Leading apps integrate with CGMs and smart glucometers to reduce manual entry errors. Tools like barcode scanners for food logging and automatic syncing also cut down on mistakes.
To maintain data integrity, many apps include real-time validation and error-checking algorithms. For instance, Logi combines meal scanners with nutritional databases to calculate glycemic loads accurately, giving users precise insights into how their food choices affect blood sugar levels.
Visual data tools, such as charts, graphs, and trend analysis, help users connect their behaviors to blood glucose outcomes. The EMPOWER-D study found that interactive data visualizations and easy entry methods significantly improved patient engagement and glycemic control.
Apps with strong tracking capabilities and user-friendly designs have shown measurable clinical benefits. Studies report HbA1c reductions ranging from 0.3% to 1.3%, along with improvements in self-management behaviors like consistent blood sugar monitoring and medication adherence.
When users can trust an app’s data accuracy and navigate its features effortlessly, they’re more likely to make informed decisions that lead to better blood sugar management and overall health improvements.
sbb-itb-0899721
Personalized Tools for Blood Sugar Control
With the foundation of clear design and precise tracking, personalized tools take blood sugar management to the next level by offering tailored strategies that fit individual needs.
These tools transform standard tracking apps into dynamic health companions by customizing feedback and recommendations based on each user's unique profile. Studies suggest that apps with personalized features can lead to better outcomes, with users seeing an average HbA1c reduction of 0.49% compared to traditional care methods.
The most impactful personalized tools focus on three essential areas: understanding how specific foods influence blood sugar, suggesting healthier alternatives, and delivering insights customized to individual patterns. This approach provides users with practical, actionable guidance that aligns with their lifestyle and health goals.
Meal Glycemic Load Scanners
Meal glycemic load scanners stand out as a key feature in modern diabetes management apps. These tools let users evaluate the glycemic impact of their meals by scanning barcodes, searching food databases, or manually entering meal components. By calculating the glycemic load (GL) of foods, users can anticipate how their meals will affect blood sugar levels before eating.
These scanners break down carbohydrates and fiber to provide instant GL calculations. This real-time feedback empowers users to make informed meal choices, reducing the guesswork and helping them avoid post-meal blood sugar spikes.
For example, Logi’s scanner simplifies this process by delivering quick GL calculations paired with clear nutritional insights. By avoiding complicated medical terminology, it makes it easier for users to understand how their food choices impact their health without needing extensive nutritional knowledge. Many users report feeling more confident about their decisions when armed with this immediate, accessible information.
Low GI/GL Food Alternatives
Another valuable feature is the ability to recommend foods with low glycemic index (GI) and glycemic load (GL), helping users maintain steadier blood sugar levels and consistent energy throughout the day. These tools guide users toward foods that result in gentler blood sugar responses, promoting better overall control.
Powered by smart AI, many of these systems analyze user preferences, dietary restrictions, and past eating habits to suggest low GI alternatives that are tailored to individual needs. Instead of providing generic food lists, these tools offer personalized recommendations that resonate with users’ tastes and lifestyles.
Logi’s Low GI/GL Food Alternatives Finder exemplifies this by offering detailed nutritional information alongside healthier food options. This feature helps users manage blood sugar, maintain a balanced weight, and sustain energy levels by suggesting alternatives that align with their preferences.
What makes these systems effective is their ability to introduce healthier options gradually, allowing users to improve their diets without feeling overwhelmed. This step-by-step approach increases adherence and supports long-term success in managing blood sugar.
Customized Health Insights
Personalized health insights tie everything together by turning user data - like blood glucose trends, meal patterns, and activity levels - into actionable advice.
These insights go beyond simply displaying numbers. They interpret the data to offer specific recommendations, such as adjusting meal timing, tweaking portion sizes, or identifying foods that frequently cause spikes. By connecting user behavior to blood sugar outcomes, these insights help users set realistic goals and make meaningful changes.
For instance, Logi’s daily meal tracking feature provides users with a clear view of their nutritional totals and patterns. This helps them form sustainable habits by linking their food choices to their blood sugar management goals.
Research shows that personalized trend analysis and feedback boost users’ confidence and motivation for self-management. Users value tools that explain the "why" behind their blood sugar trends, making it easier to adjust their routines and stay on track.
The real power of these insights lies in their simplicity. When apps present complex health data in clear, actionable formats, users are more likely to engage. Whether it’s adjusting meal timing, experimenting with new food combinations, or identifying successful habits, these tools make managing blood sugar feel achievable and rewarding.
Long-Term Tracking and Data Analysis
Long-term tracking transforms everyday health data into meaningful trends, showing how lifestyle choices influence blood sugar control over time. This broader perspective builds on the personalized insights discussed earlier, offering a deeper understanding of diabetes management.
Research highlights the benefits of apps equipped with strong tracking and analytics features. Studies reveal that individuals who consistently monitor multiple health metrics develop better self-management skills and experience improved glycemic control. By examining historical data, users can spot trends and make informed adjustments to their routines, leading to better outcomes.
Effective tracking systems focus on gathering and analyzing key data points, such as blood glucose levels, carbohydrate intake, meal glycemic loads, medication adherence, exercise, and weight changes. This multi-layered approach helps users and healthcare providers connect the dots between lifestyle choices and blood sugar fluctuations.
Long-Term Glycemic Load Tracking
Monitoring glycemic load over time provides a clear picture of how dietary habits affect blood sugar management. Unlike single-day snapshots, long-term tracking uncovers patterns and seasonal trends that might otherwise go unnoticed. For example, the EMPOWER-D study showed how an online platform that tracked diet, exercise, blood pressure, insulin use, and weight - with interactive visual tools - helped participants link lifestyle changes to blood sugar trends. This approach encouraged better self-management.
Users can identify which meals consistently maintain stable blood sugar levels and which ones lead to spikes. Tools like Logi's meal glycemic load scanner calculate the impact of meals instantly, building a detailed dietary history. Over time, this helps users understand how their overall eating habits influence blood sugar control.
Data Analysis for Behavior Patterns
Once historical data is collected, advanced analytics step in to uncover behavior patterns. These features go beyond simply displaying data - they analyze correlations between actions and blood sugar outcomes. For example, analytics might identify when spikes occur, what foods or activities preceded them, and how various factors interact to influence glycemic control. This enables users to recognize the effects of specific behaviors and adjust their routines for better results.
Visual dashboards make complex data easier to understand. Interactive charts summarizing weekly or monthly trends allow users and clinicians to pinpoint areas needing attention. Logi's daily meal tracker is a great example, offering clear views of nutritional breakdowns and eating patterns. By analyzing trends in meal timing, portion sizes, and food choices, the tool presents insights in a straightforward way, helping users make sense of their data.
Automated insights further enhance the experience by offering tailored recommendations. For instance, if a user frequently experiences spikes after certain meals, the app might suggest adjusting portion sizes or tweaking the meal composition to improve blood sugar management.
Combining multiple data sources strengthens pattern recognition. Integrating meal tracking with metrics like physical activity, sleep quality, and medication adherence reveals connections that single-variable tracking might miss. This approach highlights the interconnected nature of diabetes management.
Device integration also plays a key role in accurate and comprehensive long-term tracking. Apps that sync with continuous glucose monitors, smart insulin pens, fitness trackers, and other devices create robust datasets, making it easier to identify trends while reducing the effort required from users.
The ultimate goal of advanced data analysis is to help users build sustainable habits. By clearly showing how daily choices impact long-term outcomes, these tools guide users toward more informed decisions, leading to better blood sugar control over time.
Conclusion: What Makes Diabetes Apps Effective
Research highlights the key elements that make diabetes apps impactful. A 2025 meta-analysis of 41 studies revealed that these apps contributed to a mean reduction in HbA1c of 0.49%, compared to standard care, showing measurable improvements in blood sugar control.
The most effective apps combine reliable tracking tools with a user-friendly interface and simplified data entry. But it’s not just about having these features - it’s about how they’re designed to keep users engaged.
One standout feature is personalization, which elevates these apps beyond basic tracking tools. Features like meal glycemic load scanners and customized health insights give users the tools they need to manage their blood sugar more effectively. For instance, Logi takes this approach further by offering in-depth meal analysis and AI-driven suggestions for healthier food options.
Another critical component is device integration. According to user reviews, 43% of users cited device syncing as the most valuable feature, followed by tracking capabilities at 32.2%. Apps that seamlessly connect with continuous glucose monitors and fitness trackers not only reduce manual input but also provide a more complete picture of a user’s health.
Psychological design also plays a big role in keeping users engaged. Apps that help users understand their data foster a sense of competence, while personalized goals promote autonomy. Connectivity features, like communication tools for healthcare providers, further enhance the experience. Additionally, apps with reminders and goal-setting tools are linked to better treatment adherence.
For long-term success, sustained user engagement is essential. Apps that present complex health data in easy-to-understand visuals make it simpler for users to track progress and make informed adjustments. The best apps turn daily health data into actionable insights, empowering users to make smarter decisions over time.
In short, diabetes apps shine when they integrate accurate tracking, intuitive design, personalized features, and seamless device connectivity into a single, easy-to-use platform that fits effortlessly into daily life.
FAQs
How can diabetes apps help improve blood sugar management and lower HbA1c levels?
Diabetes apps like Logi are transforming how individuals manage their blood sugar levels and overall health. By incorporating features such as a meal glycemic load scanner, daily meal tracker, and a tool to find low GI/GL food alternatives, these apps give users the tools they need to make informed dietary decisions and monitor their progress seamlessly.
The glycemic load scanner in Logi evaluates meals by analyzing key factors like carbohydrates and fiber, helping users understand how their food choices affect blood sugar levels. Meanwhile, the daily meal tracker offers a clear view of eating habits, making it easier to spot patterns and adjust for better control. Together, these tools simplify the process of adopting healthier routines and maintaining steady energy throughout the day.
How does integrating with devices improve the functionality and user experience of diabetes management apps?
Device integration takes diabetes management apps to the next level by simplifying data collection and offering real-time insights. Imagine connecting the app to a glucose monitor or fitness tracker - suddenly, blood sugar levels, physical activity, and other health metrics are logged automatically, eliminating the need for manual entry.
This kind of integration doesn’t just save time; it also boosts accuracy and consistency in tracking. With better data at their fingertips, users can make smarter choices about their diet and lifestyle. Plus, by linking to these devices, apps can provide personalized recommendations and insights that align with each user’s specific health needs, making diabetes management more effective and user-friendly.
How do personalized insights in diabetes apps improve blood sugar management and overall health?
Diabetes apps equipped with features like meal glycemic load scanners and daily meal trackers give users the tools they need to make smarter food choices. By showing how specific meals impact blood sugar levels, these apps help users take charge of their glucose management.
Beyond immediate benefits, these tools encourage healthier long-term habits. They allow users to spot trends in their eating patterns and explore better food options. This personalized approach makes managing blood sugar more practical and consistent, boosting energy levels and supporting overall health.